
Sudden cardiac arrest (SCA) is one of the leading causes of death among adults in the United States. When cardiac arrest happens, the heart suddenly stops beating effectively. Blood flow to the brain and vital organs stops.
Without CPR, a person in cardiac arrest will not survive.
Cardiopulmonary resuscitation (CPR) keeps blood moving to the brain and heart until advanced medical care arrives. CPR includes two parts: chest compressions and rescue breaths.
Every minute that passes without CPR lowers a person’s chance of survival. Starting CPR within 3–5 minutes can significantly improve survival and reduce brain damage.
It’s completely normal to feel nervous about stepping in. Many people worry they might hurt someone or make the situation worse. But cardiac arrest is already life-threatening. Doing something is always better than doing nothing. Broken ribs can heal. A stopped heart cannot.
You are more likely to perform CPR on a family member, friend, or coworker than on a stranger. Most states have Good Samaritan laws that protect people who provide emergency care in good faith.
This course follows the 2025 Emergency Cardiovascular Care (ECC) guidelines and is designed to help you act quickly, safely, and confidently.
Course Topics Outline
When someone suddenly collapses, stay calm and move step by step.
Check the Scene
Before helping, quickly look around.
Are there dangers such as traffic, fire, exposed electrical wires, or unsafe surroundings? If the scene is not safe, do not approach. Call 9-1-1.
Your safety always comes first.
If available, use personal protective equipment (PPE) such as disposable gloves or a breathing barrier. PPE helps protect you from blood or bodily fluids. However, do not delay life-saving care if PPE is not immediately available.
Avoid direct contact with blood whenever possible and wash your hands after providing care.
Check Responsiveness
Tap the person and shout, “Are you okay?”
For an infant, gently tap the foot.
If the person does not blink, move, speak, or respond, consider them unresponsive.
Shout for help. Point directly to someone and say, “You, call 9-1-1.” Point to another person and say, “You, get the AED.” Designating someone prevents confusion.
If you are alone:
Check Breathing
Look at the chest for normal breathing for at least 5 seconds but no more than 10 seconds.
Normal breathing means steady, regular chest rise and fall.
Gasping is not normal breathing. Gasping may:
If the person is unresponsive and not breathing normally, begin CPR immediately.
ECC Chain of Survival
Survival from cardiac arrest depends on a sequence of critical actions called the Chain of Survival:
CPR follows this order:
C – Compressions
A – Airway
B – Breathing
We begin with compressions to keep blood moving.
The standard cycle for one rescuer is:
30 compressions followed by 2 breaths (30:2).
If you are not trained in rescue breaths, or do not feel comfortable giving them, perform Hands-Only CPR:
Hands-Only CPR is appropriate for sudden adult collapse. Breaths are especially important for children, infants, drowning victims, choking, or drug overdoses.
Once you determine the person is unresponsive and not breathing normally:
If you are trained to check a pulse, check for no more than 10 seconds.
If you are not trained in pulse checks, do not delay — begin compressions.
Hand Position
Give Compressions
Push hard and fast.
Remember these four things:
Rate: 100–120 compressions per minute.
Depth: At least 2 inches (5 cm), but not more than 2.4 inches.
Recoil: Let the chest fully rise between compressions.
Don’t Stop: Do not interrupt compressions for more than 10 seconds.
CPR is hard work.
If a second rescuer is available:
After 30 compressions:
Open the Airway
The tongue is the most common airway obstruction in an unresponsive person.
If you see something clearly blocking the airway and it is easy to remove, remove it. Do not perform blind finger sweeps.
Give Breaths
If the chest rises, the breath is effective.
If the chest does not rise:
Give each breath just enough to make the chest visibly rise, and avoid giving breaths too quickly or too forcefully.
Continue 30:2 cycles until:
Recovery Position
If the person starts breathing normally:
Continue until:
Children and infants often experience cardiac arrest because of breathing problems. Rescue breaths are especially important.
Child CPR
If alone and the collapse was not witnessed:
Compressions:
Airway and breaths are the same as adults.
Infant CPR
Compressions:
Airway:
Breaths:
If alone and collapse was not witnessed:
A common sign of choking is when someone grabs their neck with one or both hands. This is known as the universal choking sign.
Ask, “Are you choking?”
If they cannot speak, breathe, or cough forcefully:
Continue until the object comes out or they can breathe.
If the person becomes unconscious:
For pregnant individuals or those you cannot reach around, use chest thrusts instead.
Infant Choking
If an infant cannot cry, cough, or breathe:
If the infant becomes unconscious:
A breathing emergency is any serious problem that affects a person’s ability to breathe. It may range from shortness of breath to a complete inability to breathe, and it always requires immediate attention.
Breathing emergencies can be caused by:
Other triggers may include:
Signs and Symptoms
Watch for:
Asthma
Asthma is a common cause of breathing emergencies, especially in children. Many people with asthma know their triggers and carry a rescue inhaler.
Common triggers include smoke, dust, pets, perfume, mold, exercise, stress, or sudden temperature changes.
First Aid Steps
A choking emergency happens when something blocks the airway, making it hard or impossible to breathe. This is a serious situation that requires quick action.
What Causes Choking?
Choking can happen when a foreign object—such as food or a small item—blocks the airway. Common causes include:
Signs of Choking
A person who is choking may:
First Aid for Choking
Special Situations
If the Person Becomes Unconscious
Some emergencies affect the brain and nervous system, and others affect the heart and circulation. Either way, fast action matters.
In this chapter, you’ll learn how to recognize common warning signs and what to do until EMS arrives.
Check the Scene + Call for Help
A. Cardiac Emergency: Heart Attack
A heart attack happens when blood flow to part of the heart muscle is blocked, causing damage to heart tissue.
Common signs and symptoms may include:
First Aid steps:
B. Nervous System Emergencies
1) Stroke
A stroke happens when blood flow to the brain is blocked or when a blood vessel in the brain ruptures. It often occurs suddenly.
Signs and symptoms may include:
First Aid steps:
2) Seizure
A seizure is abnormal electrical activity in the brain. It can look like mild shaking or strong convulsions. Most seizures stop within a few minutes.
Possible causes include:
First Aid steps:
3) Head and Spinal Injuries
Head and spinal injuries can affect movement, sensation, breathing, and alertness.
Possible causes include:
Signs and symptoms may include:
First Aid steps:
If the Person Becomes Unresponsive
Definition
An allergy occurs when the body’s immune system reacts to a substance (called an allergen) that is usually harmless. An allergy emergency can happen when someone is exposed to that allergen.
Allergic reactions can become serious very quickly if not treated.
Common Causes
People may be allergic to:
Signs and Symptoms
Watch for:
Anaphylaxis
Anaphylaxis is a severe, life-threatening allergic reaction. It can happen within seconds or minutes after exposure to an allergen.
It may cause:
Anaphylaxis requires immediate medical treatment, including epinephrine and emergency medical care.
First Aid Actions
Bites and stings can happen anywhere—at home, outdoors, or at work. Most are minor, but some can cause serious infection, allergic reactions, or venom exposure. Knowing how to respond quickly can prevent complications.
Common Causes
Bite and sting emergencies may involve:
Warning Signs and Symptoms
Watch for:
Types of Bite and Sting Emergencies
Animal and Human Bites
Any bite that breaks the skin can lead to infection.
If the animal is behaving strangely (such as a bat, raccoon, skunk, or stray dog), rabies may be a concern and medical evaluation is important.
Snake Bites
If you are unsure whether a snake is venomous, treat the bite as potentially serious.
Symptoms of a venomous bite may include severe pain, swelling, nausea, vomiting, or weakness.
Insect and Arachnid Stings
Bee, wasp, spider, or scorpion stings may cause mild pain and swelling. However, severe reactions can include difficulty breathing, seizures, or loss of consciousness.
First Aid Steps for Bites and Stings
Definition
A wound is an injury to soft tissue (tissue that is not bone). Wounds are generally classified as either closed or open.
Common Causes
Wounds may result from:
Signs and Symptoms
Types of Wounds
Closed Wound
A closed wound does not break the skin. A bruise is the most common example.
More serious closed wounds can involve damage to deeper tissues, blood vessels, or muscles and may cause internal bleeding.
Open Wound
An open wound breaks the skin. It can range from minor scrapes and small cuts to deeper or more severe injuries.
Major open wounds, especially those involving heavy bleeding or amputation, require immediate medical attention.
First Aid Steps
Muscle, bone, and joint injuries happen when a body part moves in a way it should not. These emergencies can result in sprains, strains, fractures, broken bones, or dislocations.
Common causes include falls, trips, sports injuries, sudden impacts, or motor vehicle accidents.
Signs and Symptoms
Types of Injuries
Fracture (Broken Bone)
A fracture can range from a small crack to a complete break.
If the bone breaks through the skin, it is called an open fracture and requires immediate medical care.
Dislocation
A dislocation occurs when a bone moves out of its normal position at a joint. This often affects the shoulder, elbow, wrist, jaw, or hip.
Sprain and Strain
First Aid Steps
Call 9-1-1 if:
Burns are injuries to the skin—the body’s largest organ. How you treat a burn depends on how deep the damage is.
Burns can happen from:
Kitchen accidents, like touching a hot stove or spilling boiling water, are very common causes.
Signs and Symptoms
The skin may appear red, white, charred, or leathery depending on severity.
Types of Burns
What NOT to Do
First Aid Steps
An Automated External Defibrillator (AED) can help restore a normal heart rhythm.
Use it as soon as it becomes available.
Important:
If no AED is available, continue CPR.
A poison is any substance that can cause illness, injury, or death when it enters the body. Some poisons are harmful if swallowed or inhaled, while others can cause damage through skin contact.
Poisoning can happen in everyday situations.
Common Sources of Poisoning
Warning Signs of Poisoning
How Poison Enters the Body
Swallowed
The most common type. Includes food, medications, alcohol, plants, and chemicals.
Inhaled
Gases or fumes such as carbon monoxide, chlorine, paint fumes, or sewer gases.
Absorbed
Through the skin. Includes chemicals, pesticides, and poisonous plants.
Injected
From bites, stings, or needles.
What to Do
Register, complete your quiz and have your personalized certification card in your mailbox!
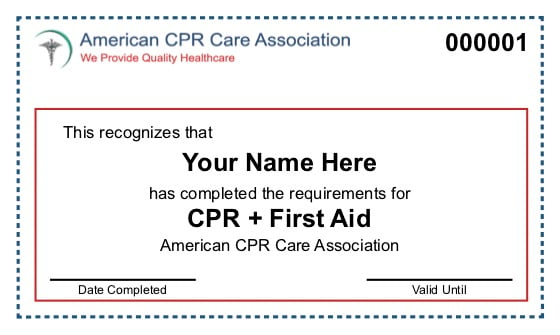
Takes less than 2 minutes to sign up.
Chapter 11: A sprain is the tearing of the ligaments at a joint. Use the RICE method when dealing with a sprain or strain.

